Table of Contents
What is collagen wound dressing? How does collagen wound dressing work?
Collagen wound dressings are sheets, sponges, plugs, films, gels and particles, which are comprised of distinct types of collagen derived from usually bovine, porcine or equine. Collagen is the most abundant proteins in the body of the vertebrates, and it is an essential substrate for cell adhesion and migration. Additionally, collagen is an important activator for platelet adhesion and aggregation after injury. Collagen wound dressing is effective in hemostasis, wound healing and regeneration.
What types of collagen dressings are best for wound healing?
There are a total of 28 different collagen types which are further divided into eight subfamilies, with the majority of the collagen types belonging to the fibril-forming or fibrillar subfamily. ref 1 This subfamily includes collagen type I and III, the most abundant components of the extracellular matrix of the dermal layer of skin. Also, the collagen types I, II, and III are the most prevalent fibrillar collagens. The unique characteristic of collagen is the presence of a triple helix that can range from the most as 96% (in collagen type I) to less than 10% (in collagen type XII). Therefore, collagen type I will be the best choice for using in collagen wound healing.
Ref. 1: Sources of Collagen for Biomaterials in Skin Wound Healing. Bioengineering 2019, 6, 56.
Type I Collagen:
Collagen type I builds a scaffold with thick fibers that serve as structural support in such as muscle, skin, tendons, vasculature, lungs, and heart, which also is constituted as the organic material in the calcified tissue such as bones and teeth. Both collagen type I and III collagens are necessary for wound healing and tissue regeneration, collagen type III plays an important role during the early phases and collagen type I is highly synthesized during the late stages.
Type II Collagen:
Collagen type II is also a fibrillar collagen, as the main component of cartilage, it is important for providing tensile strength to the tissue. Collagen type II has been used as a biomaterial in the application of bone or cartilage tissue regeneration, however, it is less known for its effect on skin wound healing.
Type III Collagen:
Collagen type III is one of dominated factors in the maturation of collagen type I, which produces thin, less durable fibers with quick turnover, however, it is less stable as compared with collagen type I. In mammals, the reticular fibers made of collagen type III is usually observed along with collagen type I.
Formats of collagen wound dressing
Preparation of collagen for use as a biomaterial can be divided into two approaches, the in-soluble and soluble collagen. The major approach in the applications of collagen wound dressings is in-soluble collagen which remains the biological structure and intermolecular linkage of inherent collagen in the human body.
Collagen wound dressings can be formed into three dimensional scaffolds in the shape of sheets, sponges, plugs, films, gels, particles, etc.
In general, the formats of collagen wound dressing like the collagen sheet, sponge, film and particles can be applied in the various epidermal or dermal wounds such as burns, traumatic wounds, surgical wounds, chronic wounds, etc.
1/ Collagen sheet wound dressing
Collagen wound dressing is normally prepared by casting and freeze drying processes, and then different shapes or dimensions can be performed by using a specific casting mold. Collagen sheet wound dressing can be used as both temporary and permanent coverings for superficial wounds related to epidermal or dermal injury. During wound healing, the ability of cellular ingrowth within a collagen wound dressing depends on the pore size and porosity of its fibrous structure. Collagen sheet wound dressing is well-suitable for burns, ulcers and surgical wounds as they revealed rapid epithelialization and dense fibrosis tissue ingrowth in the subdermal layers.
2/ Collagen particles wound dressing
Collagen particles wound dressing can be sprinkled sufficiently to cover the wound surface with irregular situation such as tunnelled wounds. Most importantly, collagen particles wound dressing can be mixed with normal saline to make a paste or a solution to be more easily applied to the wound.
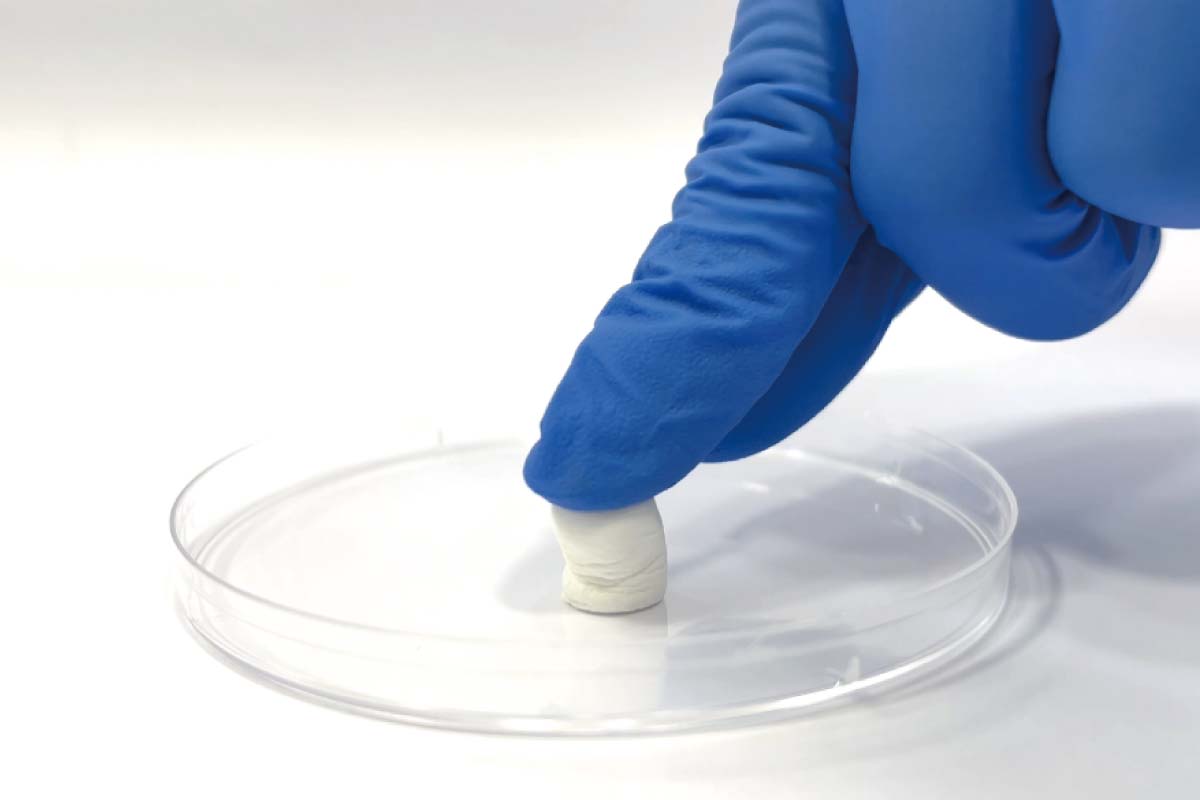
3/ Collagen plug wound dressing
In addition to the superficial wound management, the collagen wound dressing is also widely used in dentistry. Recently, the socket preservation is an effective strategy to maintain bone volume after tooth extraction. Collagen plug wound dressing is a cyindrical-shaped collagen matrix for fitting in the extraction socket, it can provide a scaffold for periosteal cells growth which is suitable for applications in bone tissue engineering.
4/ Collagen gel wound dressing
The gel form materials have become more important in wound management due to their high water content and excellent tissue adhesion. Moreover, the gel form materials are easier to incorporate active component such as antibacterial agent as compared with wound dressing shaped as a sheet or sponge. According to recent research, the collagen gel wound dressing comprised by using pure collagen, collagen blends with natural and/or synthetic polymers, or collagen blends with bioactives, and they are necessary for better management of skin wounds due to wound type diversity and environmental complexity.
Top 5 benefits of using collagen wound dressing for chronic wounds
- Collagen is the most abundant proteins in the body of the vertebrates;
- Collagen is chemotactic to cellular elements of healing such as granulocytes and fibroblasts;
- Collagen wound dressing is able to be formed as three dimensional scaffold with different specifications for distinct wound types;
- Collagen wound dressing is a porous matrix which is favorable for cellular attachment, migration and proliferation.
- Collagen wound dressing serves as an ideal substrate to promote wound maturation by alignment with native wound bed, that is, to improve quality of healing.
How long does it take for collagen wound dressing to promote healing?
Wound healing can be united into a sequence of four time-dependent phases, including:
- Coagulation and hemostasis, immediately after injury;
- Inflammation, begins shortly thereafter;
- Proliferation, starts within days of the injury;
- Wound Remodeling, in which scar tissue formation takes place, and which may last up to a year or more.
Collagen wound dressing serves as an ideal substrate to promote wound maturation by alignment with native wound bed. That is, collagen wound dressing will be effective in shortening the time course in the wound remodeling phase and thus improving quality of healing.
Can collagen wound dressing be used on infected wounds?
In the infected wounds, the inflammatory response is still at a relatively high level and the inflammatory cells will secrete various kinds of enzymes such as matrix metalloproteases (MMP) which can degrade collagen in situ. Therefore, the collagen wound dressing is not recommended to be used on infected wounds.
How often should I change the collagen wound dressing?
The treatment cycle will depend on the healing progress of the wound. Collagen is a biodegradable material, therefore there is no need to remove collagen wound dressing after using. Instead of that, following the original collagen wound dressing is degraded, repeatedly placing a new one to the wound when needed.
What factors should be considered when determining the collagen wound dressing change frequency?
Collagen wound dressing has the ability to uphold the healing process maintaining the moist environment around the wound as well as it absorbs the exudate. Therefore, a new dressing will be used if there is still a lot of exudate from the wound or the collagen wound dressing is absorbed.
Better absorption performance: Collagen hydrogel wound dressing & Collagen wound dressing with alginate
The alginate material is one of the advanced wound dressings which have significant antibacterial properties and can absorb many times its own weight in exudate. Additionally, the alginate material also has hemostatic properties but it is recommended for use in the control of minor bleeding (for example, in post-debridement wounds). That is, the alginate material will not be adequate for treatment of heavier bleeding.
On the contrary, collagen wound dressing is not only an important activator for platelet adhesion after heavier bleeding, but also serves as an ideal substrate to promote wound maturation by alignment with native wound bed. Therefore, the collagen wound dressing combined with alginate material can have the structural support of collagen and the gel-forming properties of alginate, and then to be more effective in wound management.
What is bovine collagen wound dressing?
Collagen wound dressings are made up of collagen obtained from various sources such as bovine, porcine, marine, equine and where bovine and porcine are among the most common. There is a high demand for bovine based collagen wound dressing instead of using porcine due to certain religious beliefs. Bovine collagen displays low immunogenicity and positive characteristics with limited immune response.
Can bovine collagen wound dressing be used on patients with allergies to animal products?
The collagen derived from animal tissue is biocompatible and safe in clinical use after removing the telopeptide which is a potential risk for immune response. However, it is still not recommended to use collagen wound dressing made of animal sources in the patient with severe allergy history or hypersensitive to animal derived products, such as bovine or porcine.
Are there any side effects or risks associated with using collagen wound dressing?
The collagen based biomedical products are in the form of scaffolds, haemostats, skin grafts and wound dressings. Biocompatibility, low risk of infection and low immunogenicity strongly supported the usage of collagen wound dressing in the wound management.
How to choose the best collagen wound dressing?
The best collagen wound dressing is expected to be with the following requirements:
- Non-allergenic, non-sensitizing
The collagen wound dressing is mostly prepared from animal sources, therefore the scientific verification such as the removal of telopeptide and virus inactivation during the development of collagen wound dressing will be critical on the safety in clinical use. - Highly hemostatic and moist microenvironment
One of the most important characteristics of collagen wound dressing is excellent hemostatic property contributed from platelet adhesion and exudate absorbed after heavier bleeding. Therefore, the porosity of collagen wound dressing will be the critical index for hemostatic property. In general, the porosity higher than 80% and the exudate absorbed ratio larger than 20 folds its own weight will be more suitable for clinical use.
What are contraindications for collagen wound dressing?
There is almost no contraindications for collagen wound dressings. Please do not use the collagen wound dressing on infected wounds or in the patient with severe allergy history or hypersensitive to animal derived products.
How does collagen wound dressing compare to other wound care products in terms of cost-effectiveness and patient outcomes?
There are many clinical trials being used to verify the efficacy of collagen wound dressings, it plays a remarkable role in treatment of wounds such as first-, second- and third-degree burns, diabetic foot ulcers, bed sores, surgical wounds, etc. ref 2 In a comparative study between the treatment of collagen sheet and heparin dressing against second-degree burns, it was concluded that the group treated with collagen showed better results than the group treated with heparin in terms of toleration towards the dressing and overall cost-benefit. One more comparative study between collagen dressing and paraffin gauze on 20 adult patients that require 40 cm2 of the skin by Sreekumar et al., revealed that the group treated with collagen dressing had less pain and high collagen epithelialization was observed at day 10 compared to paraffin gauze.
Ref. 2: Bovine Based Collagen Dressings in Wound Care Management. Journal of Pharmaceutical Research International 2020;32(33):48-63.